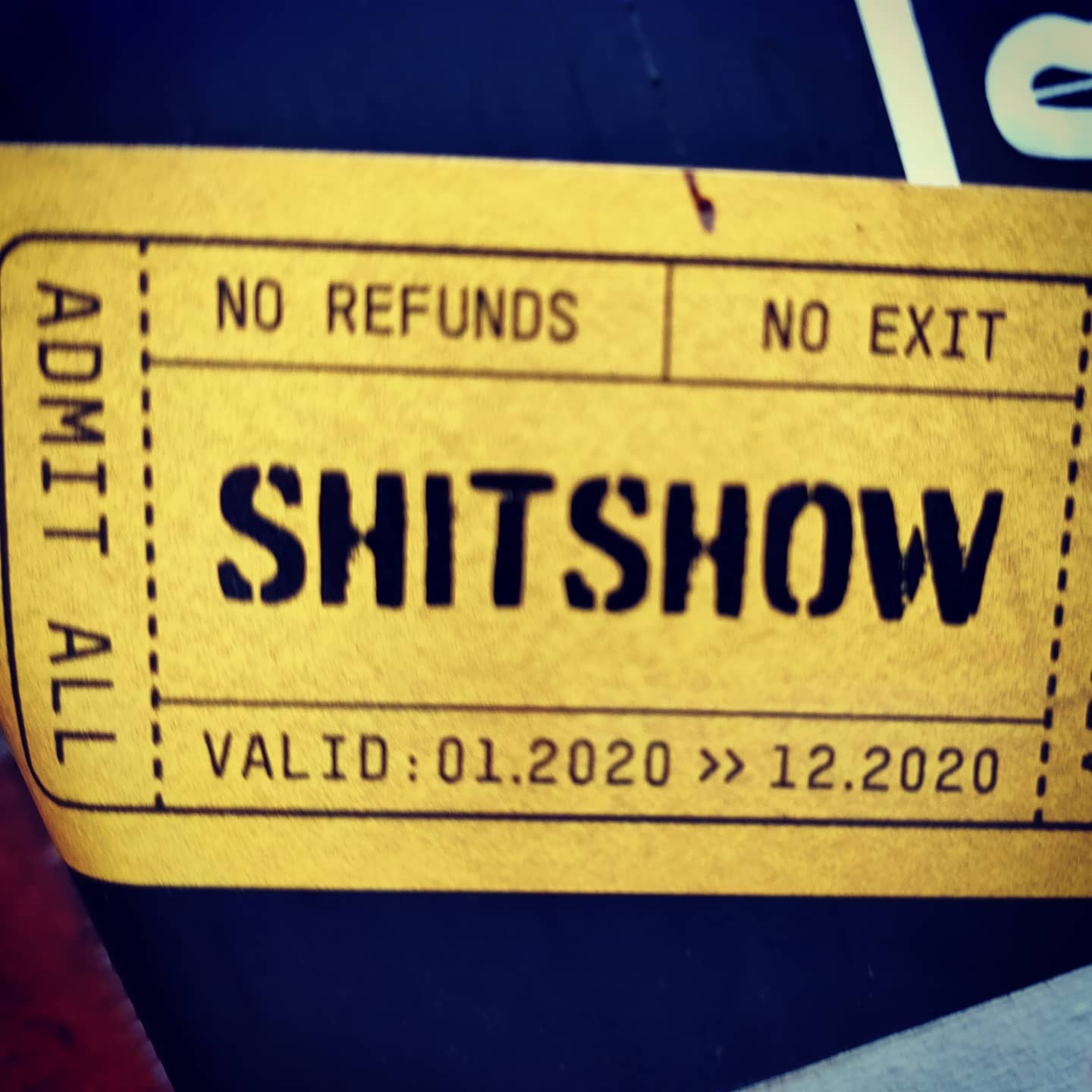
It would seem my suspicions about shared care between Gender GP and my doctors were completely correct. Yet again I’ve been let down by my doctors!
After the elation a few weeks ago that my Doctors were finally going to help, this week it’s made me realise than the help is still not forthcoming, and nothing has changed since I started this process.
Gender GP told my GP years ago I would need blood tests done at the minimum of every year.
They have done this once so far and now the doctors will not share the blood test results with Gender GP unless they write to them again and request this. Alternatively, I must collect these results and pass them on to Gender GP.
This has never been an issue when I’ve had private blood test done.
From this point on I’ll be cutting my own GP out of the loop as they’ve had my blood test results each time off my care provider.
My doctors have also told me today my Oestradiol and Testosterone levels are normal? Normal for what?
It took me 20 minutes for them to give me the levels over the phone. 0.9nmol/L for Testosterone and 101pmol/L for Oestradiol. Which is on the low side. I know this because I’ve been paying for blood tests every quarter for the past 3 years and its always been between 142 and 207 for over 18 months.
I was so right not to wait for the NHS and do my own care, and after this fuck up, I’ll be doing the same again next quarter.
Next step is to get my Gender Recognition Certificate completed, my GP to sign it and then once that’s done I can fuck off to a more Trans friendly GP.
The irony of the doctors surgery not willing to help me so now I am self-medicating and thats not supposed to happed under NHS guidelines especially as I am under the care of a Gender Identity service, albeit not an NHS one because the waiting time is not over 5 years from date of referral!
NHS Guidelines
In March 2016 the General Medical Council (GMC) published Guidance for Doctors Treating Transgender Patients. This guidance reiterates the advice previously set out by NHS England in SSC 1417; and also explains the legal protection against discrimination and harassment given to trans people by The Equality Act 2010 and Gender Recognition Act 2004.
General Practitioners should co-operate with the specialist Gender Identity Clinics and prescribe hormone therapy (feminising or virilising endocrine therapy) recommended for their patients by the Gender Identity Clinic. The specialists at the Gender Identity Clinic make recommendations for the prescription and monitoring of these therapies but they do not directly prescribe them, or provide physical and laboratory monitoring procedures for patients.
The decision on whether or not to provide long-term feminising or virilizing endocrine therapy requires the skills of a gender specialist physician, usually working within a Gender Identity Clinic.
Typical drugs recommended by Gender Identity Clinics include oestradiol preparations (e.g. transdermal oestradiol gels and patches, and oral oestradiol preparations), testosterone preparations (e.g. gels, and Sustanon® and Nebido® injection), gonadotropin releasing hormone analogues and depilatory agents (e.g. Vaniqa®); this list is not exhaustive. Apart from Sustanon®, there are no licensed products with an approved indication for the treatment of gender dysphoria. There is, however, extensive clinical experience of the use of these products in the treatment of gender dysphoria over decades, which provides evidence of tolerability and safety comparable with their use for approved indications. The prescription of licensed products outside their approved indications, often but not always at the recommendation of a specialist provider, is not uncommon in general practice.
General Practitioners should collaborate with Gender Identity Clinics in the initiation and on-going prescribing of hormone therapy, and for organizing blood and other diagnostic tests as recommended by the Gender Identity Clinics.
General Practitioners are also expected to co-operate with Gender Identity Clinics in patient safety monitoring, by providing basic physical examinations (within the competence of General Practitioners) and blood tests and diagnostic tests recommended by the Gender Identity Clinic. Hormone therapy should be monitored at least 6 monthly in the first 3 years and yearly thereafter, dependent on clinical need.
The Gender Identity Clinic is expected to assist General Practitioners by providing relevant information and support, including the provision of guidance regarding the interpretation of blood test results
British Medical Association guide for dealing with patients with Gender Dysphoria
I also love this article, parts copied below, on the British Medical Association website: https://www.bma.org.uk/advice-and-support/gp-practices/gp-service-provision/managing-patients-with-gender-dysphoria
Be mindful of the sensitivity of their condition and of how difficult it might have been for your patient to seek treatment.
Yeah, that didn’t happen!
Be particularly mindful of medical confidentiality, when addressing your patient in person and in written correspondence.
Yeah, that didn’t happen either and my GP are still dead naming me now
Avoid misattributing commonplace health problems to gender.
They refuse to look at me as someone who has had 2.5 years worth of HRT and look solely at me as male.
Assist those patients who wish to change their personal details on their practice medical record.
Thats the best one. Despite having 2 copies of my deed pool in person and one via emails my GP still dead names me.
Inform your patient of any gender-specific disease prevention and organ screening programmes, including offering information on how to opt out and discuss any future family plans and fertility treatments options.
Nope, nothing!
Refer early to a reputable NHS GIC (gender identity clinic).
You mean like an NHS approved service where the waiting list is many years long? How many people either kill themselves, self harm or give up because they are unable to access Gender services?
Get informed about prescribing medicines that you are not normally familiar with.
My GP haven’t spoke to me once about this